Breast cancer is the most common cancer and the leading cause of cancer deaths among women worldwide. In 2020 alone, over two million women were diagnosed – that’s one in every four new cancer diagnoses. And sadly, nearly 700,000 women lost their lives to it. Many people are not fully aware of the impact of lifestyle and environmental factors on breast cancer risk.
Now, it’s interesting how it affects different parts of the world. We see more diagnoses in developed countries, but thanks to early detection and better treatments, death rates started to go down. On the flip side, women in less developed countries have much lower incidence rate, but their risk of dying is much higher because they often don’t get diagnosed until it’s too late, and they may not have access to the care they need.
The tricky part? Breast cancer cases are rising everywhere. Developed countries are seeing an alarming rise in diagnoses among younger women, and in regions where it used to be less common, like South America, Africa, and Asia. It is estimated that by 2040, we could see nearly 3 million new cases each year. A 31% jump from 2020 numbers.
The substantial variation in breast cancer rates across different countries and communities underscores the role of environmental factors in its development. High-quality and long-term studies have concluded that the genetic factors responsible for developing breast cancer account only for 5 to 10% of all cases, which means that a staggering 90 to 95% of all cases are due to environmental and lifestyle factors.
Interestingly, immigrants moving from countries with lower cancer incidence to countries with higher cancer rates soon acquire the higher risk of their new country, which further confirms the environmental impact on the disease development.
What do we mean by “Environment”?
The environment encompasses everything that’s not genetic, including social, built, and chemical aspects. The social environment, built environment, and toxicologic or chemical environment all play a role in breast cancer risk.
- Built Environment: The physical surroundings where people live, work, and play can impact their health. Access to healthy food options, green spaces, and opportunities for physical activity can all influence breast cancer risk.
- Social Environment: Socioeconomic status, family structures, and early-life experiences can influence breast cancer risk.
- Toxicologic and Chemical Environment: Exposure to various chemicals, both natural and synthetic, can contribute to breast cancer development.
Breast cancer risk, what does the evidence say?
Before diving into details on all the various environmental risk factors that you could try to mitigate or reduce your exposure too, lets explore in short an extremely important study called the TWO sisters study, which included 2 sub studies conducted by the National Institute of Environmental Health Sciences (NIEHS);
Study A
The first study is called the Sister Study, involving over 50,000 women, and is the larger of the two. It focuses on how lifestyle, environment, biology and genetics contribute to breast cancer development. By comparing women who developed breast cancer with their unaffected sisters, researchers have uncovered several key findings:
- Biological Aging: As age is a major risk factor, researches have discovered that biological aging, which is a measure of DNA changes, is linked to environmental exposures and the higher likelihood of developing breast cancer.
- Vitamin D: Regular vitamin D supplements were linked to lower rates of breast cancer in postmenopausal women.
- Hair Dye: Regular hair dye use was associated with around 9% increased breast cancer risk for all women. However, that incidence jumped to a whooping 60% increased chance of developing breast cancer when it comes to black women using permanent dyes every five to eight weeks or more, in comparison to 8% increased risk for white women with similar use.
- Exercise: Women who were active in their youth (ages 5-19) had a lower risk of breast cancer later in life.
- Air Pollution: Exposure to higher levels of lead, mercury, and cadmium increased the risk of postmenopausal breast cancer.
- Sleep Problems: Poor sleep (four or more nights per week) was associated with increased breast cancer risk.
- Diabetes during Pregnancy: Women who developed diabetes during multiple pregnancies had a higher breast cancer incidence.
Study B
The second NIEHS study focuses on young-onset breast cancer (before age 50). This research has identified several biological factors that may reduce the risk of early-onset breast cancer:
- Older age at the start of menstruation (menarche)
- Younger age at menopause
- Premenopausal hysterectomy (removal of the uterus)
- Early age at first pregnancy
Additionally, this study has shed light on the impact of chemicals on breast cancer risk:
- Endocrine Disruptors: Exposure to endocrine-disrupting chemicals during key life stages (prenatal, puberty, pregnancy, menopause) may increase breast cancer risk.
- Chemicals and Puberty Timing: Exposure to high levels of chemicals like triclosan (found in antimicrobial soap) was associated with early breast development in girls, while exposure to benzophenone-3 (found in sunscreen) was linked to delayed breast development.
- Chemical Screening: Roughly 300 common chemicals were found to affect hormones linked to increased breast cancer risk. These chemicals are found in various products that we use regularly and may also be present in air and water pollution.
Now let’s further explore these environmental and life style factors so we can have an understanding of how to mitigate the risk for everyone, but particularly for those who are at a high risk due to age, family history, or history of other reproductive cancers such as ovarian or uterine cancer. Mitigating these risk factors may also help in reducing the chance of recurrence for those who already had it, or even potentially slow down the progression of the cancer for those who are currently going through treatment.
Breast Cancer Risk Factors or Exposures Influenced by the Environment and Human Choices and Behaviors
Exogenous Hormones
Breast cancers can be sensitive to estrogen and progesterone in the body. Pathologists examine cancer cells for hormone receptors, which the cells use to absorb estrogen or progesterone for growth. If a cancer is estrogen receptor-positive (ER-positive) or progesterone receptor-positive (PR-positive), hormone therapy can block growth. Cancers lacking these receptors (HR-negative) don’t respond to hormone therapy.
Some breast cancer cells have too much of a certain protein called HER2. While healthy breast cells make some HER2, these cancer cells make much more. Lab tests can determine if breast cancer cells have extra HER2 and using drugs that damage cells with excess HER2 (targeted therapy), can help control this type of breast cancer. Unfortunately, there are a small percentage of breast cancer cases that are triple negative (ER, PR, and HER2 negative), these cancers are more aggressive, often affecting younger women, and they much harder to treat. Triple negative breast cancer is strongly associated to certain gene mutations (BRCA1, BRCA2).
That being said, approximately 80% of breast cancers are hormone receptor-positive. Therefore, factors that impact the natural levels of estrogen and progesterone in the body can significantly influence the risk of developing breast cancer.
Hormone-based birth control and hormone replacement therapy (HRT) may elevate the risk of a number of cancers. These hormones, similar to the body’s natural estrogen and progesterone, can stimulate cancer growth, particularly in breast tissue. They may also make cervical cells more susceptible to the human papillomavirus (HPV), increasing the risk of cervical cancer.
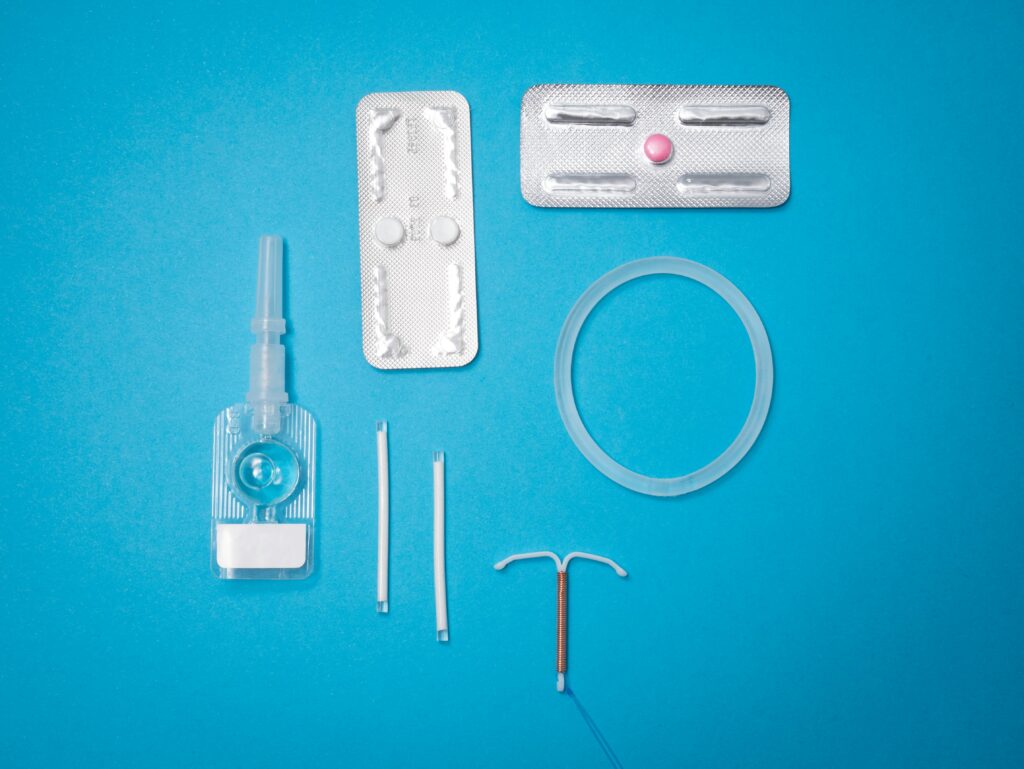
Hormone-based birth control:
A recent study by the Cancer Epidemiology Unit at Oxford Population Health, has revealed that any type of hormonal contraception increases the risk of breast cancer.
The study analyzed data from 9,498 women between the ages of 20 and 49 who had developed invasive breast cancer, comparing them with 18,171 closely matched women without breast cancer. It was found that about 44% of women with breast cancer and 39% of those without had a prescription for a hormonal contraceptive an average of three years prior to the diagnosis, with about half of these being prescribed a progestogen-only contraceptive.
The research team calculated the association between using different types of hormonal contraceptives and the risk of breast cancer and the key findings from the study include:
- A significant increase in breast cancer risk was associated with the use of hormonal contraceptives, whether they were progestogen-releasing intra-uterine device (32%), progestogen-only oral contraceptives (26%), combined oral contraceptives (estrogen and progestogen) 23%, injected progestogen (25%).
- The combined analysis with previous studies confirmed an increased risk of breast cancer in current and recent users of all types of progestogen-only contraceptives.
The increased risk associated with oral contraceptives decreased after stopping their use.
The researchers estimated that the absolute excess risk of developing breast cancer over 15 years with five years of oral contraceptive use varied with age. It ranged from 8 additional cases per 100,000 women for use between ages 16-20, jumping up to 265 additional cases per 100,000 women for use between ages 35-39.
This confirms the results of a previous large Danish study in 2017 showed about 20% increase in breast cancer risk for women using or recently stopping combined hormone OCs, varying depending on the specific type (0% to 60%) and duration of use.
Hormonal replacement therapy (HRT):
When it comes to HRT in post-menopausal women, the findings were as alarming. A 2002 important US study, called the Women’s Health Initiative (WHI), tracked 161,809 postmenopausal women aged 50 to 79 between 1993 and 1998. This study found an increased risk of breast cancer, heart disease, stroke, and blood clots in participants. These findings have been supported by subsequent research.
A 2020 UK large study, involving 98,611 women aged 50-79 diagnosed with breast cancer between 1998 and 2018 and 457,498 similar women without breast cancer, examined HRT use. 34% of the breast cancer group and 31% of the control group had used HRT. The study found that current HRT use (within five years) increased breast cancer risk. Estrogen-only therapy increased the risk by 15%, while combined estrogen and progestogen therapy increased it by 79%.
The risk varied depending on the type of progestogen used, with norethisterone posing the highest risk (88% increase) and dydrogesterone the lowest (24% increase). Past long-term use of combined estrogen-progestogen therapy also increased risk (16% increase). The study estimated that current estrogen-only therapy could lead to 3 to 8 additional breast cancer cases per 10,000 women per year, while current combined therapy could lead to 9 to 36 additional cases. Past long-term combined therapy might result in 2 to 8 extra cases.
The impact is much worse for those who had a previous history of breast cancer. A 2022 analysis of four studies with 4,050 patients investigated HRT’s impact on breast cancer survivors. Half of the participants received HRT (either combined estrogen/progestogen or tibolone), while the other half received a placebo or no HRT. HRT significantly increased the risk of breast cancer recurrence compared to the placebo (46% increase). This increased risk was primarily seen in patients with hormone receptor-positive breast cancers (80% increase), not in those with hormone receptor-negative cancers. The analysis concluded that HRT is detrimental for breast cancer survivors, especially those with hormone receptor-positive disease, and suggested exploring alternative treatments for menopause symptoms.
Diethylstilbestrol (DES):
Also known as stilbestrol or stilboestrol, is a synthetic estrogen, used until 1971 to prevent miscarriages, but unfortunately has a devastating long-term effects. Daughters exposed in utero have increased rates of reproductive abnormalities, including a higher risk of breast cancer, especially after age 50. This confirms the critical impact of exposures during pregnancy and how it affects the baby’s development.
Lifestyle factors
Obesity:
Being overweight or obese has many causes, including our surroundings. It’s been known for a while that body mass index (BMI) can affect breast cancer risk differently depending on when a woman goes through menopause. A higher BMI is linked to increased risk after menopause but not as clear link before menopause.
However, BMI might not be the best way to measure body fat. Abdominal fat, the kind around your middle, could be more important for things like insulin resistance and cancer risk. The different breast cancer risks before and after menopause might be because of the types of tumors that are more common in each group.
After menopause, tumors that respond to estrogen are more frequent, and fat tissue produces estrogen then. Before menopause, tumors that don’t respond to estrogen are more common and might have different risk factors. Fat tissue can also store certain chemicals called EDCs, which can stay in the body for a long time and might contribute to obesity themselves. Scientists are still trying to figure out why the link between obesity and breast cancer changes throughout a woman’s life.
Physical Activity:
Physical activity, particularly in postmenopausal women, has a protective effect against breast cancer, likely by reducing body fat and estrogen levels.
Tobacco:
Both active and secondhand smoke increase risk. The numerous carcinogens in tobacco can be found in breast tissue of smokers. The risk is higher for those starting young and those with certain genetic traits affecting carcinogen metabolism.
Alcohol:
Alcohol consumption is a well-documented risk factor for breast cancer, reduce or eliminate your alcohol consumption, particularly if you are at a high risk.
Diet:
Diet plays a significant role in breast cancer risk.

- Western Diet: A large meta-analysis of over 43,000 cases highlighted the impact of dietary patterns. The “Western” diet, high in energy, red and processed meats, and animal fats, was linked to a 14% increased risk, while the “prudent” diet, rich in fruits, vegetables, and whole grains, was associated with an 18% decreased risk. These effects varied by menopausal status. The Western diet’s increased risk was mainly seen in postmenopausal women, likely due to increased estrogen levels from fat tissue after menopause. The prudent diet’s protective effect was stronger in premenopausal women, whose naturally higher estrogen levels may be more responsive to dietary changes. The Western diet was also linked to a higher risk of hormone-sensitive tumors, while the prudent diet seemed protective against both hormone-sensitive and insensitive tumors, potentially due to its high content of phytoestrogens, antioxidants, and folate. Carotenoids, the pigments in colorful fruits and vegetables, have shown anticarcinogenic properties. A 20-year observational study found that women with higher carotenoid blood levels had an 18-28% lower breast cancer risk and a significantly lower risk of recurrence and death, suggesting protection against aggressive cancers. However, carotenoids are best obtained from food, not supplements, as some studies have linked beta-carotene supplementation to increased lung cancer risk in smokers.
- Vitamin D’s role is complex. Large observational studies suggest a link between vitamin D deficiency and increased breast cancer risk, with higher vitamin D levels associated with lower risk. These studies also observed that vitamin D supplementation, particularly in postmenopausal women, may lower the risk. However, clinical trials haven’t shown a significant risk reduction with vitamin D supplements, possibly due to their shorter duration.
- Vitamin C link to breast cancer risk has been inconclusive, although initially thought to reduce the risk significantly, a 2022 rigorous research study divided into 2 sub studies, one following over 88,000 women for over 30 years, and another following 93,000 women for over 20 years, found no link between vitamin C intake (from supplements, food, or combined) and breast cancer risk. That being said, vitamin C, a known antioxidant, might still be important in breast cancer treatment. It could boost the effects of chemo and radiation, or, in few cases, high-dose intravenous vitamin C therapy has been used alone, with varying success, for those who can’t or won’t have conventionanl treatments. This specific therapy involves regular intravenous injections of high doses. For more information on this, check out my other article on holistic breast cancer treatments.
- Soy consumption has been debated, but safety evaluations haven’t revealed significant risks. Soybeans contain isoflavones, which can bind to estrogen receptors, potentially lowering excess estrogen and protecting against breast cancer. Studies suggest isoflavones may also inhibit breast cancer cell growth. A 2022 meta-analysis found a significant inverse relationship between soy isoflavone intake and breast cancer risk in both pre- and post-menopausal women, with higher intake linked to lower risk. Soy isoflavones were also inversely associated with recurrence risk. A 2015 review concluded that soy-rich diets were associated with a 25% reduction in recurrence risk and a 15% reduction in mortality among women with the disease. It’s important to note that properly prepared soy is safe for consumption, as heat treatment eliminates compounds that could affect digestion. Soy allergy is also relatively rare.
Certain Environmental exposures
Multiple harmful environmental exposures have been linked to increased risk of developing breast cancer!
Radiation:
Such as that used in medical imaging like CT scans and mammograms, is a well-established risk factor for breast cancer, particularly when exposure occurs early in life. The risk is present even at low doses, and it’s estimated that medical radiation may contribute to about 1% of annual breast cancer diagnoses in the U.S. While these procedures are often medically necessary, it’s crucial to ensure their appropriate use and minimize radiation exposure whenever possible.
Exposure to light at night:
Which can disrupt the body’s natural circadian rhythms often linked to shift work, increases risk, possibly by suppressing melatonin, which has anti-estrogenic effects. This is concerning given the high number of women in night shift jobs. Sources of light at night include shift work, ambient lighting, electronic devices, and travel across time zones.
Metals:
While heavy metals are primarily linked to lung cancer, some like lead and cadmium have estrogenic properties and have been associated with breast cancer. Lead exposure has also been linked to delayed puberty.

Endocrine Disrupting Chemicals (EDCs):
Primarily in Personal Products can mimic or disrupt hormones, particularly estrogen signaling, and are found in many consumer products.
- Phthalates: Phthalates are chemicals used in plastics and cosmetics. Some phthalates have been associated with breast cancer and early breast development in limited studies.
- Parabens: Parabens are preservatives in personal care products that can act like weak estrogens. They have been detected in human urine and breast cancer specimens.
- Bisphenol A (BPA): BPA is a weakly estrogenic chemical found in plastics and epoxy resins. It can leach into food and beverages and has been detected in human urine samples. While animal studies have shown increased risk, more human studies are needed to confirm the degree of risk.
- Other EDCs: Polybrominated diphenyl ethers (PBDEs) and perfluoroalkyl substances (PFASs) are other EDCs that have been detected in human samples and may have implications for breast cancer risk, although more research is needed.
Industrial and Agricultural Chemicals
- Benzene: Benzene is an industrial chemical classified as a human carcinogen. It has been linked to an increased risk of breast cancer in women.
- Polychlorinated Biphenyls (PCBs): PCBs were used in various industrial applications until they were banned. Studies have shown inconsistent results regarding their association with breast cancer, but there is evidence of a gene-environment interaction increasing risk.
- Ethylene Oxide: Ethylene oxide is used for medical equipment sterilization and has been classified as a carcinogen. Studies suggest an increased risk of breast cancer among exposed workers.
- Dioxin: Dioxin is a highly toxic chemical that is persistent in the environment. Limited studies suggest a possible association with breast cancer, particularly with higher exposure levels and longer follow-up periods.
- 1,3-Butadiene: This chemical, found in petroleum products and cigarette smoke, is a carcinogen. While no studies have specifically examined its effect on breast cancer in humans, animal studies show an increase in mammary tumors.
- Pesticides: Exposure to pesticides, particularly DDT, during early development may increase breast cancer risk. Studies in adults have shown inconsistent results.
- Air Pollution and Polycyclic Aromatic Hydrocarbons (PAHs): Air pollution contains various carcinogens, including PAHs, which have been linked to breast cancer. Studies have shown associations between air pollution exposure and breast cancer risk, particularly for ER+/PR+ tumors.
Drinking Water Contaminants:
Contaminants in drinking water, such as disinfection byproducts, pesticides, and heavy metals, have been the subject of numerous studies examining their potential link to breast cancer.
Dietary Contaminants:
Including those from industrial sources, food packaging, and high-temperature cooking methods, have also been investigated in relation to breast cancer risk.
The low down
As women, we understand the anxieties surrounding breast cancer. While some risk factors are unavoidable, the good news is that the majority of cases are linked to environmental and lifestyle factors – things we can control. This knowledge empowers us! Reducing your risk involves minimizing exposure to air pollution and harmful chemicals found in plastics, personal care products including hair dyes containing Phenylenediamin(pdd), and even certain foods. Opt for fresh, whole foods, and consider organic options when possible.
And of course, unless absolutely necessary with no other alternative, try to avoid the use of Hormone-based birth control and hormone replacement therapy, particularly if you are at high risk.
Maintaining a healthy weight, staying active, avoiding smoking or being around smokers, and limiting alcohol consumption are also crucial.
Eat more colorful vegetables and fruits, avoid deep fried, fatty and processed foods, and unless you are allergic, increase your intake of soy foods such as soy milk, tofu and tempeh. Checkout the diet section
I know these changes aren’t always easy. But even small steps can make a big difference. Prioritize sleep, manage stress, and find healthy ways to unwind.
Finally, while we can work to minimize risks, early detection remains vital. Regular self-exams, mammograms, and discussions with your doctor are essential. Early detection significantly improves treatment outcomes. By understanding the risks and making positive changes, you’re taking control of your health journey.

